Abstract
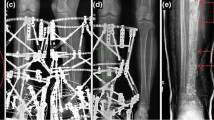
As the demand for limb-sparing surgeries after wide resection of bone lesions reaches an all-time high, so does the need for durable reconstruction. Recent advances in distraction osteogenesis within the field of orthopedic oncology have shown promising outcomes, offering the ability to restore near-normal function and reduce complications associated with non-biological constructs. The aim of this study is to identify, describe, and summarize the techniques, indications, and outcomes of the Ilizarov method for the management of bone tumors. The relevant literature describing the use of distraction osteogenesis in orthopedic oncology was identified from appropriate electronic databases (PubMed, MEDLINE, CINAHL, and EMBASE), and a narrative review was undertaken. Methods of distraction osteogenesis were classified into two groups: external and internal fixation. Within each group, we outline the indications and surgical techniques for several precise methods of distraction based on patient factors (age, psychological considerations) and tumor characteristics (proximity to the joint, location, type, and size of tumor, + / − radiation therapy/chemotherapy). We also report on various considerations and complications and highlight the pitfalls and benefits associated with each technique. Despite the potential of long duration of fixation, the frequency of pin-tract infections, and the technical expertise required, distraction osteogenesis allows for the regeneration of living bone with sufficient biologic affinity, biomedical strength, and resistance to infection. Given that the complications can be prevented or minimized, the use of distraction osteogenesis is likely to expand as the primary method of reconstruction in orthopedic oncology.


Similar content being viewed by others
Data Availability
Not applicable.
Code Availability
Not applicable.
Change history
16 June 2023
A Correction to this paper has been published: https://doi.org/10.1007/s42399-023-01509-w
References
Tsuchiya H, et al. Safety of external fixation during postoperative chemotherapy. J Bone Joint Surg Br. 2008;90(7):924–8.
Matsubara H, Tsuchiya H. Treatment of bone tumor using external fixator. J Orthop Sci. 2019;24(1):1–8.
Hosny GA. Limb lengthening history, evolution, complications and current concepts. J Orthop Traumatol. 2020;21(1):3.
Lesensky J, Prince DE. Distraction osteogenesis reconstruction of large segmental bone defects after primary tumor resection: pitfalls and benefits. Eur J Orthop Surg Traumatol. 2017;27(6):715–27.
Khalifa ARH. Ilizarov bone transport with knee arthrodesis in the treatment of giant cell tumor of proximal tibia. J Am Sci 2014;10(3):1–5. http://www.jofamericanscience.org.
Borzunov DY, Balaev PI, Subramanyam KN. Reconstruction by bone transport after resection of benign tumors of tibia: a retrospective study of 38 patients. Indian J Orthop. 2015;49(5):516–22.
Puri A. Limb salvage in musculoskeletal oncology: recent advances. Indian J Plast Surg. 2014;47(2):175–84.
Fox EJ, et al. Long-term followup of proximal femoral allografts. Clin Orthop Relat Res. 2002;397:106–13.
Hornicek FJ, et al. Factors affecting nonunion of the allograft-host junction. Clin Orthop Relat Res. 2001;382:87–98.
Lord CF, et al. Infection in bone allografts. Incidence, nature, and treatment. J Bone Joint Surg Am. 1988;70(3):369–76.
Mankin HJ, et al. Osteoarticular and intercalary allograft transplantation in the management of malignant tumors of bone. Cancer. 1982;50(4):613–30.
Raskin KA, Hornicek F. Allograft reconstruction in malignant bone tumors: indications and limits. Recent Results Cancer Res. 2009;179:51–8.
Oh CS, et al. Bone transport for reconstruction in benign bone tumors. Clin Orthop Surg. 2015;7(2):248–53.
Atallah R, et al. Complications of bone-anchored prostheses for individuals with an extremity amputation: a systematic review. PLoS ONE. 2018;13(8):e0201821.
Watanabe K, et al. Over 10-year follow-up of functional outcome in patients with bone tumors reconstructed using distraction osteogenesis. J Orthop Sci. 2013;18(1):101–9.
KahlerOlesen U. Plate-assisted segmental bone transport with a lengthening nail and a plate : a new technique for treatment of tibial and femoral bone defects. Unfallchirurg. 2018;121(11):874–83.
Liu Y, et al. Complications of bone transport technique using the Ilizarov method in the lower extremity: a retrospective analysis of 282 consecutive cases over 10 years. BMC Musculoskelet Disord. 2020;21(1):354.
Yushan M, et al. Bifocal or trifocal (double-level) bone transport using unilateral rail system in the treatment of large tibial defects caused by infection: a retrospective study. Orthop Surg. 2020;12(1):184–93.
Bari M, Shahidul I. Trifocal bone transport by Ilizarov technique for large post-traumatic tibial bone defects: a single centre BARI-ILIZAROV experience of 46 cases. MOJ Orthop Rheumatol. 2020;1(12):12–4.
Borzunov DY. Long bone reconstruction using multilevel lengthening of bone defect fragments. Int Orthop. 2012;36(8):1695–700.
Tsuchiya H, et al. Limb salvage using distraction osteogenesis. A classification of the technique. J Bone Joint Surg Br. 1997;79(3):403–11.
Canadell J, San-Julian M. Pediatric bone sarcomas: epiphysiolysis before excision. London: Springer; 2009.
Ferchaud F, et al. Reconstruction of large diaphyseal bone defect by simplified bone transport over nail technique: a 7-case series. Orthop Traumatol Surg Res. 2017;103(7):1131–6.
Hattarki R, Bhagat S, Patel K, Singh B, Mehendiratta D, Pote R. Comparative study between intramedulary interlock nailing and plating in distal metaphyseal fractures of tibia. Surgery. Curr Res. 2016;6(3):2161–1076.
Rozbruch R, Blyakher. Lengthening and then nailing (LATN) of the tibia. in Hospital for Special Surgery Annual Alumni Meeting. 2002. New York, New York
Zhang Y, et al. Double-level bone transport for large post-traumatic tibial bone defects: a single centre experience of sixteen cases. Int Orthop. 2018;42(5):1157–64.
Zhang Q, et al. Femoral nonunion with segmental bone defect treated by distraction osteogenesis with monolateral external fixation. J Orthop Surg Res. 2017;12(1):183.
Li Y, et al. Efficacy comparison of double-level and single-level bone transport with Orthofix fixator for treatment of tibia fracture with massive bone defects. Int Orthop. 2020;44(5):957–63.
Tiefenboeck TM, et al. Pitfalls in automatic limb lengthening – first results with an intramedullary lengthening device. Orthop Traumatol Surg Res. 2016;102(7):851–5.
Farsetti P, et al. Lower limb lengthening over an intramedullary nail: a long-term follow-up study of 28 cases. J Orthop Traumatol. 2019;20(1):30.
Muratori F, Scoccianti G, Beltrami G, Matera D, Capanna R, Campanacci DA. Is an intramedullary nail a valid treatment for limb-length discrepancy after bone tumor resection? Case descriptions. Surg Technol Int. 2018;33:281–8.
Rozbruch RS, et al. Limb lengthening and then insertion of an intramedullary nail: a case-matched comparison. Clin Orthop Relat Res ®. 2008;466(12):2923–32.
Bernstein M, Fragomen A, Rozbruch SR. Tibial bone transport over an intramedullary nail using cable and pulleys. JBJS Essent Surg Tech. 2018;8(1):e9.
Quinnan SM, Lawrie C. Optimizing bone defect reconstruction-balanced cable transport with circular external fixation. J Orthop Trauma. 2017;31(10):e347–55.
Yang Z, et al. Bone transport for reconstruction of large bone defects after tibial tumor resection: a report of five cases. J Int Med Res. 2018;46(8):3219–25.
Emara KM, Ghafar KA, Al Kersh MA. Methods to shorten the duration of an external fixator in the management of tibial infections. World J Orthop. 2011;2(9):85–92.
Kocaoglu M, et al. Complications encountered during lengthening over an intramedullary nail. J Bone Joint Surg Am. 2004;86(11):2406–11.
Paley D, et al. Femoral lengthening over an intramedullary nail. A matched-case comparison with Ilizarov femoral lengthening. J Bone Joint Surg Am. 1997;79(10):1464–80.
Burghardt RD, et al. Tibial lengthening over intramedullary nails: a matched case comparison with Ilizarov tibial lengthening. Bone Joint Res. 2016;5(1):1–10.
de Souza AMG, BispoJúnior RZ. Osteochondroma: ignore or investigate? Rev Bras de Ortop (English Edition). 2014;49(6):555–64.
Baumgart R, Hinterwimmer S, Krammer M, Mutschler W. Zentrale Zugseilsysteme--vollautomatische, kontinuierliche Kallusdistraktion zur Behandlung langstreckiger Knochendefekte [Central cable system--fully automatic, continuous distraction osteogenesis for the lengthening treatment of large bone defects]. Biomed Tech (Berl). 2004;49(7–8):202–7. German. https://doi.org/10.1515/BMT.2004.038.
Kucukkaya M, Armagan R, Kuzgun U. The new intramedullary cable bone transport technique. J Orthop Trauma. 2009;23(7):531–6.
Nho SJ, Helfet DL, Robert Rozbruch S. Temporary intentional leg shortening and deformation to facilitate wound closure using the Ilizarov/Taylor spatial frame. J Orthop Trauma. 2006;20(6):419–24.
Hernandez-Irizarry R, et al. Intentional temporary limb deformation for closure of soft-tissue defects in open tibial fractures. J Orthop Trauma. 2021;35(6):e189–94.
Lerner A, Fodor L, Ullmann Y. Acute temporary malpositioning for dealing with extensive tissue loss after severe high-energy trauma to extremities. In: Kocaoğlu M, Tsuchiya H, Eralp L, editors. Advanced Techniques in Limb Reconstruction Surgery. Berlin, Heidelberg: Springer; 2015.
Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res ®. 1990;250:81–104.
Xu SF, et al. Successful management of a childhood osteosarcoma with epiphysiolysis and distraction osteogenesis. Curr Oncol. 2014;21(4):e658–62.
Kapukaya A, et al. Technique and complications of callus distraction in the treatment of bone tumors. Arch Orthop Trauma Surg. 2006;126(3):157–63.
Banfi A, et al. High-dose chemotherapy shows a dose-dependent toxicity to bone marrow osteoprogenitors. Cancer. 2001;92(9):2419–28.
Gutowski CJ, Basu-Mallick A, Abraham JA. Management of bone sarcoma. Surg Clin North Am. 2016;96(5):1077–106.
Sheplan LJ, Juliano JJ. Use of radiation therapy for patients with soft-tissue and bone sarcomas. Cleve Clin J Med. 2010;77(Suppl 1):S27–9.
Rohde RS, et al. Complications of radiation therapy to the hand after soft tissue sarcoma surgery. J Hand Surg Am. 2010;35(11):1858–63.
Tsuchiya H, et al. Distraction osteogenesis after irradiation in a rabbit model. J Orthop Sci. 2005;10(6):627–33.
Costa S, Reagan MR. Therapeutic irradiation: consequences for bone and bone marrow adipose tissue. Front Endocrinol (Lausanne). 2019;10:587.
Sun R, et al. Indirect effects of X-irradiation on proliferation and osteogenic potential of bone marrow mesenchymal stem cells in a local irradiated rat model. Mol Med Rep. 2017;15(6):3706–14.
von Eisenhart-Rothe R, et al. Primär maligne Knochentumoren. Orthopade. 2011;40(12):1121–42.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68(1):7–30.
Jacobs N, Stubbs DA, McNally MA. Ilizarov distraction osteogenesis for reconstruction of long bone defects following primary malignant bone tumour resection. Int J Orth. 2019;2(2):58–68.
Harris NL, et al. Osteogenic sarcoma arising from bony regenerate following Ilizarov femoral lengthening through fibrous dysplasia. J Pediatr Orthop. 1994;14(1):123–9.
Hillmann A, Gösling T. Gutartige Knochentumoren. Unfallchirurg. 2014;117(10):873–82.
Lam Y. Bone Tumors: Benign Bone Tumors. FP Essent. 2020;493:11–21.
Thorey F, et al. Muscle response to leg lengthening during distraction osteogenesis. J Orthop Res. 2009;27(4):483–8.
Iacobellis C, Berizzi A, Aldegheri R. Bone transport using the Ilizarov method: a review of complications in 100 consecutive cases. Strategies Trauma Limb Reconstr. 2010;5(1):17–22.
Feleke M, et al. Single-cell RNA sequencing reveals differential expression of EGFL7 and VEGF in giant-cell tumor of bone and osteosarcoma. Exp Biol Med (Maywood). 2022;247(14):1214–27.
Feng W, et al. Single-cell RNA sequencing reveals the migration of osteoclasts in giant cell tumor of bone. Front Oncol. 2021;11: 715552.
Papakostidis C, Bhandari M, Giannoudis PV. Distraction osteogenesis in the treatment of long bone defects of the lower limbs: effectiveness, complications and clinical results; a systematic review and meta-analysis. Bone Joint J. 2013;95-B(12):1673–80.
Antoci V, et al. Axial deformity correction in children via distraction osteogenesis. Int Orthop. 2006;30(4):278–83.
Ozaki T, et al. High complication rate of reconstruction using Ilizarov bone transport method in patients with bone sarcomas. Arch Orthop Trauma Surg. 1998;118(3):136–9.
Ugaji S, et al. Patient-reported outcome and quality of life after treatment with external fixation: a questionnaire-based survey. Strateg Trauma Limb Reconstr. 2021;16(1):27–31.
Liu Q, et al. A comparative study of bone union and nonunion during distraction osteogenesis. BMC Musculoskelet Disord. 2022;23(1):1053.
Green SA, et al. Management of segmental defects by the Ilizarov intercalary bone transport method. Clin Orthop Relat Res. 1992;280:136–42.
Alzahrani MM, et al. The effect of altering the mechanical loading environment on the expression of bone regenerating molecules in cases of distraction osteogenesis. Front Endocrinol (Lausanne). 2014;5:214.
Picci P, et al. Risk factors for local recurrences after limb-salvage surgery for high-grade osteosarcoma of the extremities. Ann Oncol. 1997;8(9):899–903.
Wang W, et al. Bone transport using the Ilizarov method for osteosarcoma patients with tumor resection and neoadjuvant chemotherapy. J Bone Oncol. 2019;16: 100224.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Literature review was performed by Lilly Groszman and Dr. Anas Nooh. The first draft of the manuscript was written by Lilly Groszman and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
No ethical approval is required. We completed a traditional literature review on previously published peer reviewed studies to construct a review of the most important and critical aspects of the current knowledge of this topic.
Conflict of Interest
The authors declare no conflict of interest.
Disclaimer
Source of funding did not play a role in the investigation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised to correct the first paragraph of the Abstract section.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Groszman, L., Nooh, A., Bernstein, M. et al. The Ilizarov Method for the Management of Bone Tumors in the Lower Extremity: Techniques, Indications, and Outcomes. SN Compr. Clin. Med. 5, 139 (2023). https://doi.org/10.1007/s42399-023-01477-1
Accepted:
Published:
DOI: https://doi.org/10.1007/s42399-023-01477-1